COVID Patterns


Scientists, policymakers and healthcare workers are eager to discern to what extent COVID-19 may be seasonal. Understanding this aspect of the disease could guide our response to the pandemic.
Researchers at UC Santa Barbara have found evidence that the spread of COVID-19 is sensitive to UV exposure. While this suggests that COVID-19 may vary with the seasons, there are other seasonal factors — such as temperature, specific humidity and precipitation — whose effects are uncertain given the available data. The results appear in the Proceedings of the National Academy of Sciences.
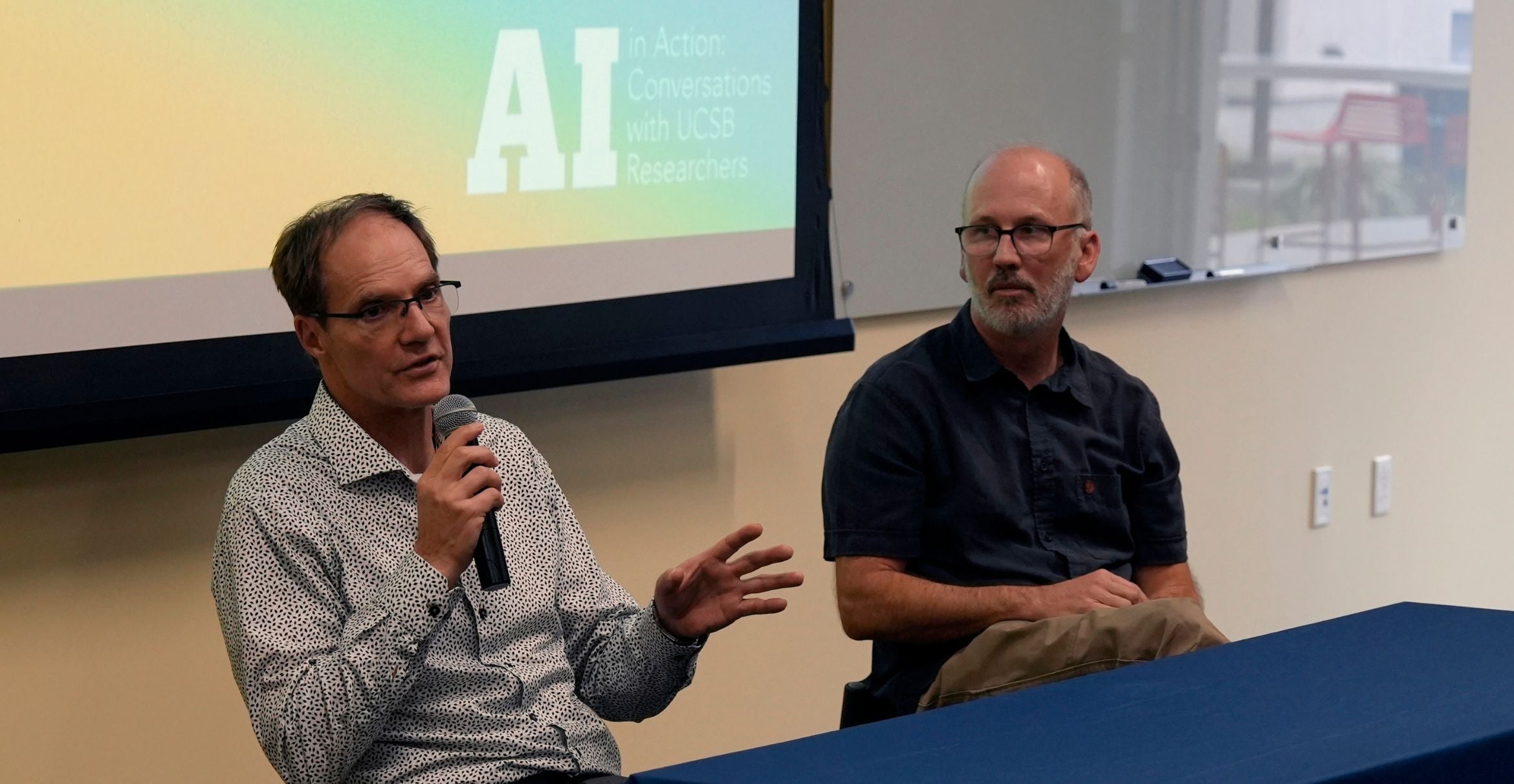
“Related species of coronavirus — like SARS from 2003 and MERS from 2012 — turned out to have weak relationships with temperature and humidity, but were sensitive to UV radiation,” said coauthor Kyle Meng, an environmental economist in UC Santa Barbara’s economics department and at the campus’s Bren School of Environmental Science & Management.
Meng, together with Tamma Carleton, also at the Bren School, Peter Huybers and Jonathan Proctor from Harvard, and Jules Cornetet at France’s École Normale Supérieure Paris-Saclay, sought to explore the relationship between UV radiation and the spread of COVID-19 by constructing a high-resolution global dataset of daily COVID-19 cases.
Many papers compare different locations to get a sense of how the disease reacts to various environmental conditions. But this approach introduces a host of potentially confounding factors into statistical models, such as health care quality, income and cultural norms.
Meng offers the more temperate United States and more tropical Brazil as examples. “The U.S. and Brazil are different for all kinds of reasons,” he said. “They have different economic conditions and institutions in addition to different environmental conditions.” These distinctions, he said, prevent a clean comparison of the spread of COVID-19 based solely on environmental conditions.
To circumvent this issue, the team conducted a longitudinal study, essentially comparing many populations to themselves over time. So, rather than compare Brazil to the U.S., they would compare communities within Brazil to themselves at a different time, when local environmental conditions changed. “We basically ask whether daily fluctuations in environmental conditions experienced by a population affect new COVID-19 cases up to two weeks later,” Meng explained.
To accomplish this, the researchers needed a lot of data. Unfortunately, when the team began their work, international COVID-19 datasets, like that of John’s Hopkins, provided data only at the country level. Records with finer resolution were scattered across different agencies and institutions in a variety of languages and formats.
“We took many disparate datasets from different countries’ statistical agencies and harmonized them to create a global dataset composed of over 3,000 spatial units,” Carleton said. The authors then used a dataset of meteorological conditions with daily resolution to match local environmental conditions to daily COVID-19 case counts.
The researchers applied a suite of statistical techniques to analyze how four variables — UV radiation, temperature, humidity and precipitation — correlated with the daily growth rate of COVID-19 cases, a measure for how rapidly the disease was spreading in a region. They also estimated the lag time between changes in environmental conditions and possible effects on recorded COVID cases, which could be significant given the virus’s four to seven-day incubation period along with additional delays due to testing.
The team found evidence that a location’s UV exposure significantly affects COVID-19 transmission. A change in UV exposure by 1 standard deviation (roughly equal to the difference in UV between May and June in Los Angeles) reduced the growth rate of new cases by around 1 percentage point over the following two weeks. That could bring down COVID-19 growth rates from an average daily increase at the beginning of the epidemic of 13% to a 12% increase per day.
Based on the expected seasonal changes in UV radiation, the model predicted growth rates would increase by 7.3 percentage points for southern temperate locations between January and June. Meanwhile, northern temperate regions would see a UV-driven decrease of 7.4 percentage points during that same period, as longer days increased UV exposure.
This pattern switches as the seasons flip. By December, the researchers predicted COVID-19 growth rates could decrease by 7.7 percentage points in southern temperate regions, compared with July numbers, while cooler northern areas could see a jump of 7.8 percentage points over this period.
Importantly, the seasonal influence of UV on transmission of the disease is small relative to that of social distancing policies such as travel bans, school closures or home isolation, the authors noted. Regardless of the weather, social distancing measures appear to be necessary to substantially slow the spread.
Conforming with these findings, infection rates appear to have decreased in the northern hemisphere during the summer, possibly due to increased UV exposure. However, much of the northern hemisphere also relaxed their COVID stay-at-home orders at the same time, Meng said. As a result, there’s a conflation between UV effects and the loosening restrictions during the summer months. “This is a big reason why our study uses daily fluctuations in UV exposure, in part to avoid conflating influences when looking at long-term, varying fluctuations.”
These findings are consistent with concerns about the surge of COVID-19 infections currently being experienced in the U.S. with the arrival of winter; however, to get the full seasonality picture, researchers will need more precise estimates of how the disease responds to other seasonally varying environmental conditions, such as temperature and specific humidity. “We are confident of the UV effect, but this is only one piece of the full seasonality picture,” Carleton said.
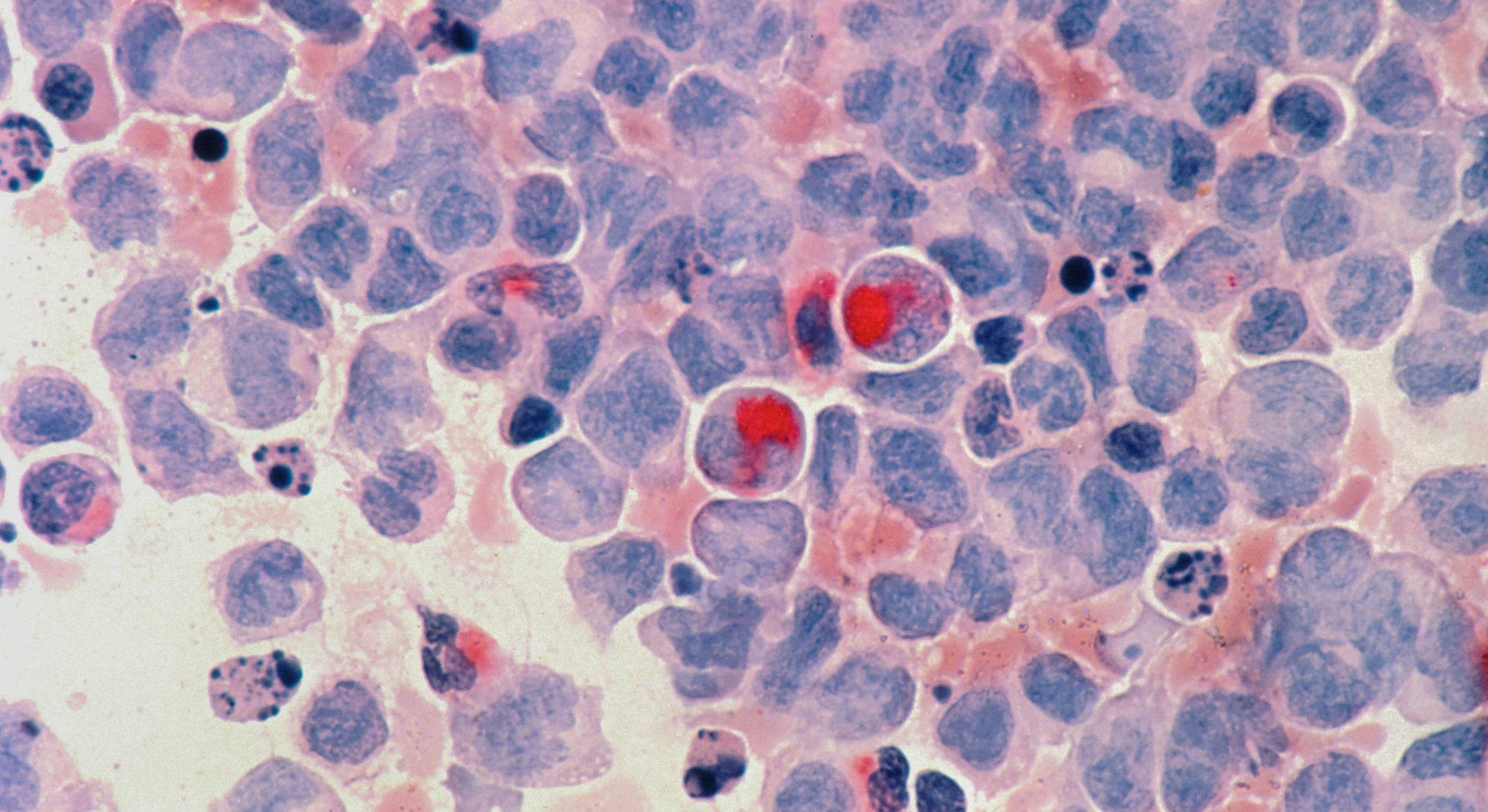
Lab studies will ultimately be critical in determining the mechanisms at work, though the authors suspect multiple factors may be behind the effect of UV on COVID-19 transmission, some of which cannot be studied in the lab. The first is biological. UV can damage the nucleic acids that the virus uses to encode its genetic information. Coauthor Jonathan Proctor, a post-doctoral fellow at Harvard, posited that UV radiation may inactivate the virus as it is being transmitted, such as when it’s suspended in the air or resting on an exposed surface. “Just as UV can destroy our own DNA if we don’t use sunscreen, UV can damage the COVID-19 virus,” Proctor said.
Another component is behavioral. For example, people may go out more often when it is sunnier, which could alter the risk of transmission. While laboratory studies can help determine the biological mechanisms, population-level studies like this one are able to also capture social factors.
“In the context of all this, our study suggests that seasonal changes in UV may influence COVID-19 transmission in the coming months,” Meng said. “And if that’s true, we need to think carefully about how to modulate COVID-19 containment policies in a seasonal manner.”