Aerosols vs. Droplets
Winter is on its way. And in this year of coronavirus, with it comes the potential for a second wave of COVID-19. Add in flu season and our tendency to head inside and close our windows to the cold, wet weather, and it appears the next several months are going to present us with new health challenges.
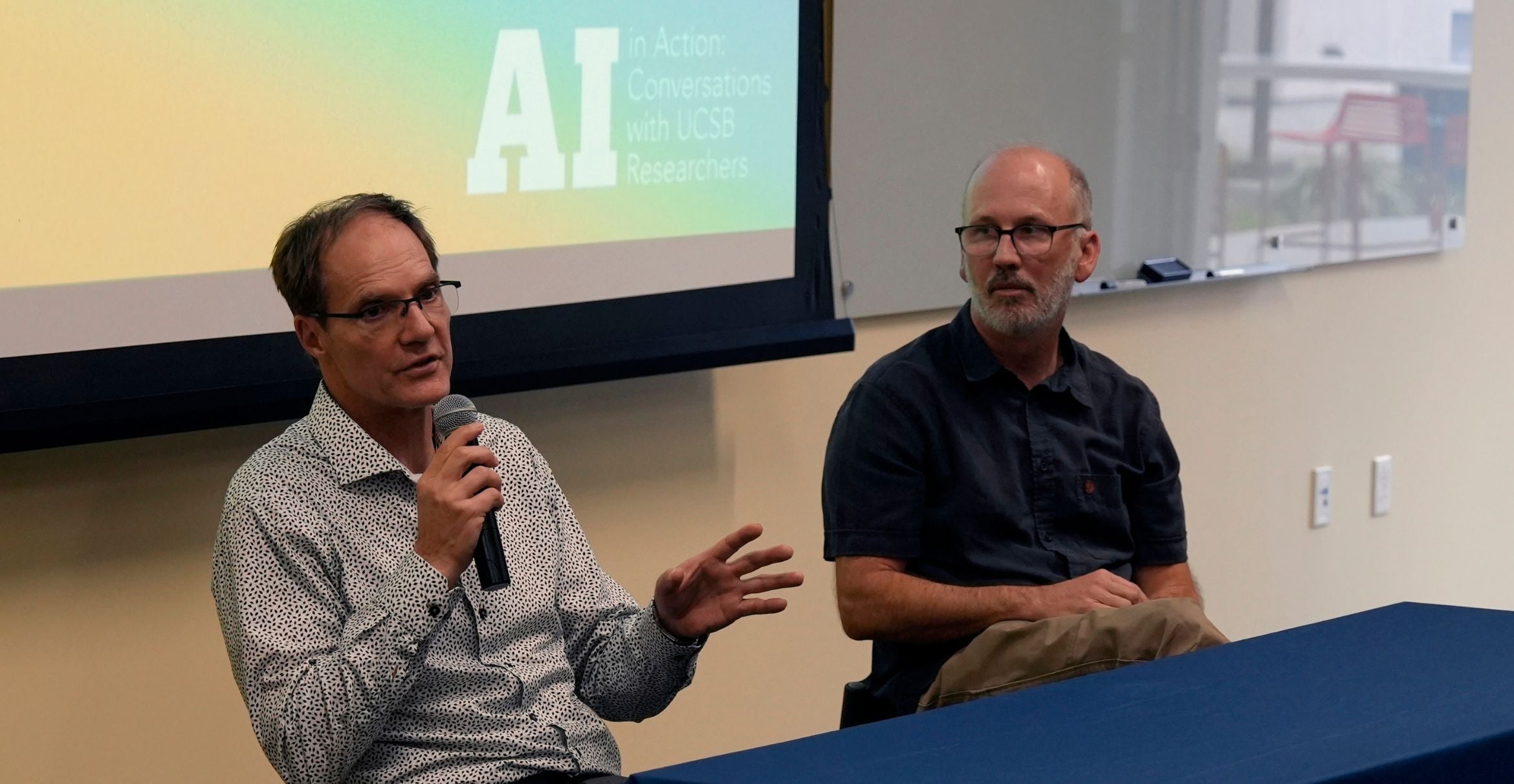
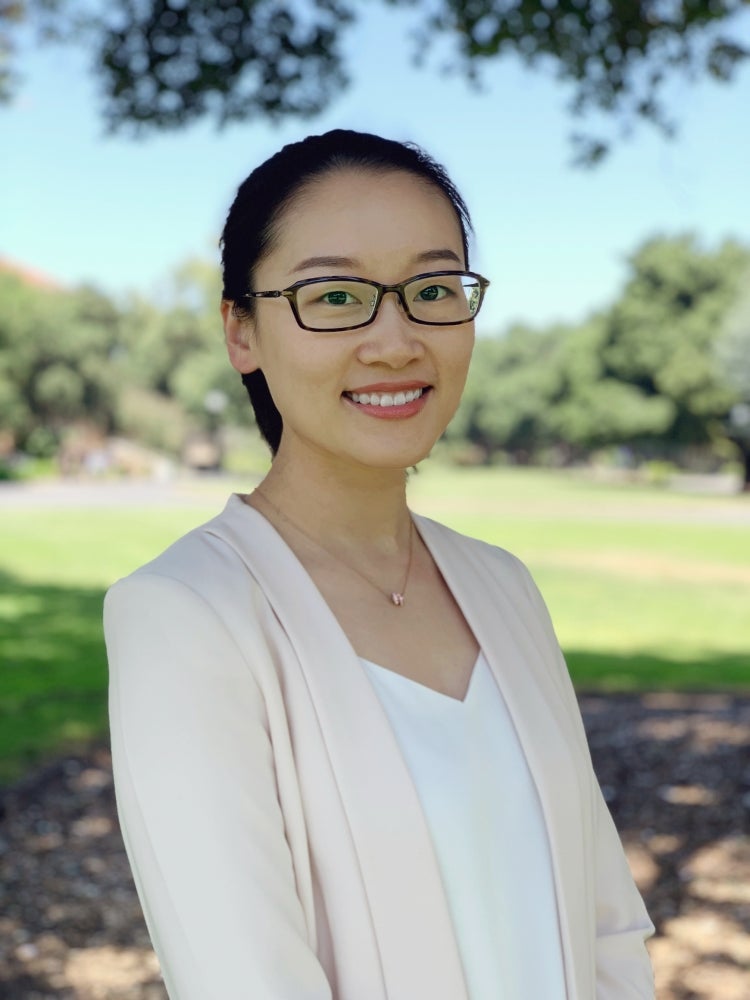
UC Santa Barbara researchers Yanying Zhu and Lei Zhao hope to arm people with better knowledge of how SARS-CoV-2 spreads as the seasons change. Their new study investigates the secret of this virus’s unusual success: its transmissibility, or how it manages to get from host to host. The dominant mode, it turns out, changes according to environmental conditions.
“Back at the beginning of April a lot of people were wondering if COVID would go away in the summer, in the warmer weather,” said Zhu, a professor of mechanical engineering and one of the authors of a paper that appears in the journal Nano Letters. “And so we started to think about it from a heat transfer point of view, because that’s what our expertise is.”
The virus, of course, did not disappear during the summer as hoped, and in fact COVID cases across the country continued to climb. To understand how the novel coronavirus manages to persist in circumstances in which the flu virus fails, Zhu, Zhao and colleagues modeled different temperatures and relative humidities along a continuum from hot and dry to cold and humid in typical indoor spaces, where the virus is distributed by normal speech and breathing — and, according to the paper, where people “only sneeze or cough into a tissue or their elbows.” To these scenarios they added emerging knowledge about the highly contagious microbe; in particular, how long it remains infectious outside a host.
The results are sobering. For one thing, respiratory droplets — the most common mode of transmission — don’t obey our social distancing guidelines.
“We found that in most situations, respiratory droplets travel longer distances than the 6-foot social distance recommended by the CDC,” Zhu said. This effect is increased in the cooler and more humid environments to distances of up to 6 meters (19.7 feet) before falling to the ground in places such as walk-in refrigerators and coolers, where temperatures are low and humidity is high to keep fresh meat and produce from losing water in storage. In addition to its ability to travel farther, the virus is particularly persistent in cooler temperatures, remaining “infectious from several minutes to longer than a day in various environments,” according to several published studies.
“This is maybe an explanation for those super-spreading events that have been reported at multiple meat processing plants,” she said.
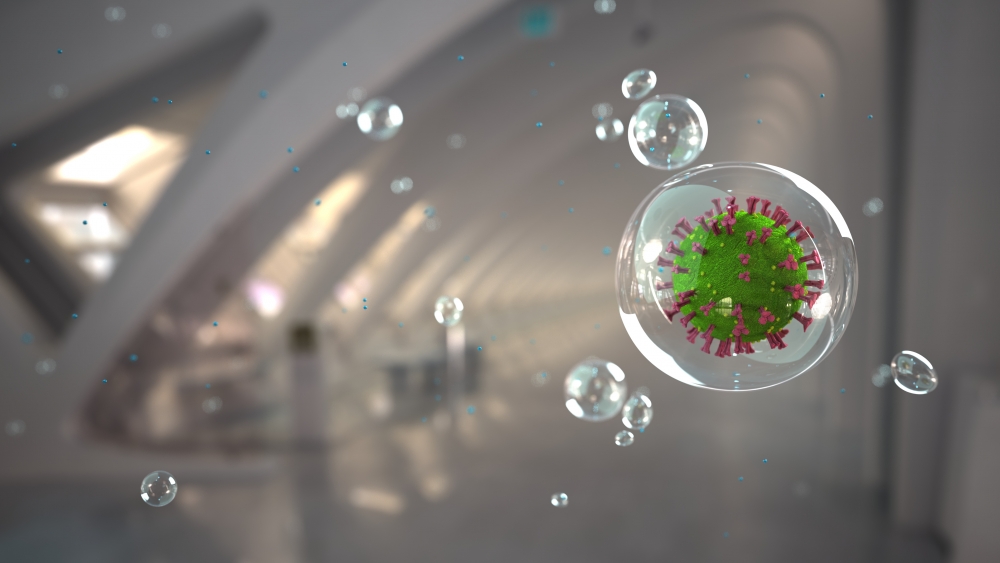
At the opposite extreme, where it is hot and dry, respiratory droplets more easily evaporate. But what they leave behind are tiny virus fragments that join the other aerosolized virus particles that are shed as part of speaking, coughing, sneezing and breathing.
“These are very tiny particles, usually smaller than 10 microns,” said lead author Lei Zhao, who is a postdoctoral researcher in the Zhu Lab. “And they can suspend in the air for hours, so people can take in those particles by simply breathing.
“So in summer, aerosol transmission may be more significant compared to droplet contact, while in winter, droplet contact may be more dangerous,” he continued. “This means that depending on the local environment, people may need to adopt different adaptive measures to prevent the transmission of this disease.” This could mean, for example, greater social distancing if the room is cool and humid, or finer masks and air filters during hot, dry spells.
Hot and humid environments, and cold and dry ones, did not differ significantly between aerosol and droplet distribution, according to the researchers.
The quantitative descriptions of virus propagation under varying local conditions could serve as useful guidance for decision-makers and the general public alike in our efforts to keep the spread to a minimum.
“Combined with our study, we think we can maybe provide design guidelines for the optimal filtering for facial masks,” said Zhao, adding that the research could be used to quantify real exposure to the virus — how much virus could land on one’s body over a certain period of exposure. This knowledge could, in turn, lead to better strategies for airflow and ventilation to prevent virus accumulation. In addition, the insights, according to the study, “may shed light on the course of development of the current pandemic, when combined with systematic epidemiological studies.”
Research on this paper was conducted also by Yuhang Qi and Prof. Paolo Luzzatto-Fegiz at UC Santa Barbara, and Prof. Yi Cui at Stanford University.