Tracking a Killer

A major cause of human disability and death throughout the world, sepsis is a condition that begins with an infection, progresses rapidly and can set off a chain of effects that result in multiple organ failure and irreparable damage to the body. Because of the condition’s rapid onset, physicians must respond immediately to the symptoms with broad-spectrum antibiotics for infection, drugs to combat inflammation and, in the more critical cases, vasopressors to manage shock.
Because sepsis is so difficult to detect in its early stages, however, little has been known about how it develops. This may explain why no new effective drugs to treat sepsis have been developed in decades, while it remains one of the leading causes of hospital deaths. Sepsis also can result in serious disabilities for those who survive.
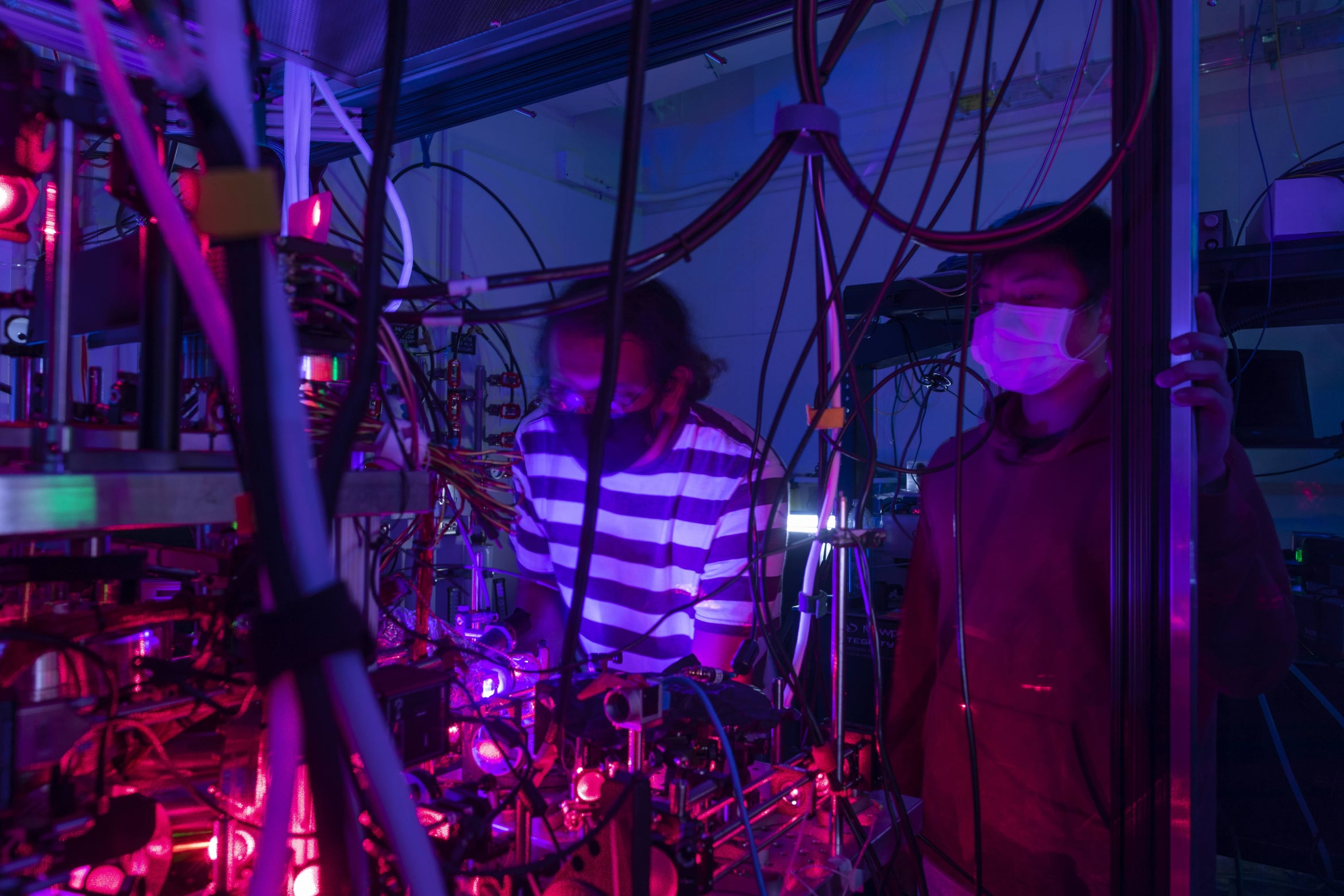
Now, researchers at UC Santa Barbara, Sanford Prebys Medical Discovery Institute (SBP) in La Jolla, California, and UC San Diego have developed a method for tracking, on a molecular level, the development of sepsis. Their resulting discoveries could, in turn, lead to more advanced therapies for sepsis that reduce its mortality, minimize the lifelong effects for survivors or even prevent the cascade of life-threatening effects before it begins, while reducing the billions of dollars spent every year to treat the condition.
Their paper, “Accelerated Aging and Clearance of Host Anti-inflammatory Enzymes by Discrete Pathogens Fuels Sepsis” is published in the journal Cell Host & Microbe.
“Sepsis is generally thought of as one singular disease, especially as it enters late stages,” said UC Santa Barbara biology professor Jamey Marth, who is the director of the campus’s Center for Nanomedicine, in addition to being a professor at SBP. “At this point, inflammation and coagulopathy have caused the vascular and organ damage common to severe sepsis and septic shock. Our comparative approach to monitor the onset and progression of sepsis at the molecular level supports the view that there are different molecular pathways in sepsis depending on host responses to different pathogens.”
An improved sepsis model yields important findings
In contrast to previous experimental models of sepsis, which typically release multiple and incompletely identified pathogens into the bloodstream, Marth and his team developed a more quantitative method that tracked the pathogen and host over time, beginning with infection. This method generated a reproducible protocol that allowed the scientists to map host responses, in this case to five different human pathogens representing common strains and isolates from different patients.
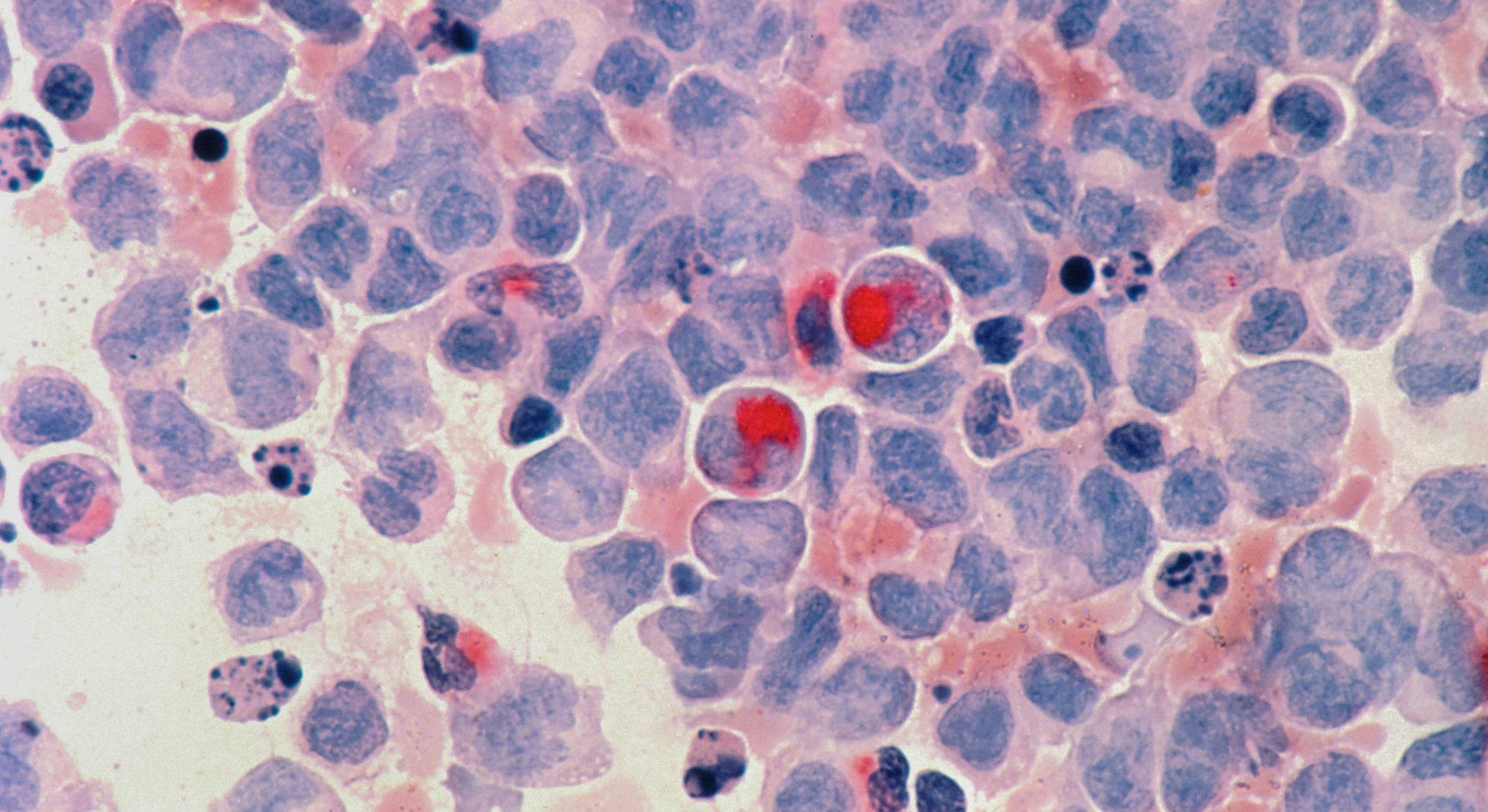
In the study, Marth’s team found that in the onset and progression of sepsis caused by Salmonella or E. coli, a protective mechanism normally present in the host was disabled. The mechanism that the bacteria used included a means to accelerate the molecular aging and clearance of two anti-inflammatory alkaline phosphatase (AP) enzymes, called TNAP and IAP, which are normally present in the host bloodstream. This was achieved through pathogen activation of the host’s own Toll-like receptor-4 (TLR-4), and both pathogens were thus able to induce inflammatory compounds and reduce the likelihood of host survival.
The scientists found that boosting the level of protective anti-inflammatory AP activity or using neuraminidase inhibitors to block the downstream effect of TLR-4 activation on NEU1 and NEU3 induction were both highly therapeutic approaches as inflammatory markers were reduced and host survival increased — indicating a potential direction for drug development.
“It has been known that AP isozymes can reduce inflammation in the context of some diseases and pathogens — indeed AP is currently in clinical trials focused on inflammatory diseases, including colitis and sepsis,” said Won Ho Yang, Ph.D., lead author and a senior scientist in the Marth laboratory at both UCSB and SBP. “This study shows that the pathogen is interacting with the host to disable a protective response. The findings also demonstrate how both pathogen and host battle each other by altering the rates of protein aging and clearance — which itself is a newly discovered regulatory mechanism we recently reported that controls the half-lives of proteins in the blood.”
In contrast, these responses weren’t seen in infections caused by other bacteria tested, including methicillin-resistant Staphylococcus aureus (MRSA) and Streptococcus pneumoniae. The different host responses in this case appeared divided between Gram-positive and Gram-negative bacteria, which describes the existence or absence of an inflammatory compound found on Gram-negative strains.
“We are continuing to map and compare host responses to different pathogens in sepsis, using state-of-the-art technical approaches, and hope to ultimately stratify the disease,” said Marth, who is the Carbon Professor of Biochemistry and Molecular Biology at UC Santa Barbara, as well as the Mellichamp Chair of Systems Biology. “It’s possible that sepsis is similar to cancer, in that we now know that cancer is a not a single disease but represents hundreds of diseases at the molecular level.”
p.p1 {margin: 0.0px 0.0px 0.0px 0.0px; font: 12.0px 'Times New Roman'; color: #000000; -webkit-text-stroke: #000000} span.s1 {font-kerning: none}
Research on this project was also conducted by Douglas M. Heithoff, Peter V. Aziz, Benjamin Haslund-Gourley and Michael J. Mahan, SBP and UC Santa Barbara; Julia S. Westman, Sonoko Narisawa, Anthony B. Pinkerton and José Luis Millán, SBP; and Victor Nizet, M.D., UC San Diego.
Research reported in this press release was supported by National Institutes of Health (NIH) Heart, Lung, and Blood Institute (HLBI) grants HL125352 and HL131474. Additional support was provided by the Swedish Research Council 2017-00192 and the Wille Family Foundation.
p.p1 {margin: 0.0px 0.0px 0.0px 0.0px; font: 12.0px 'Times New Roman'; color: #0000ff; -webkit-text-stroke: #0000ff} span.s1 {font-kerning: none; color: #000000; -webkit-text-stroke: 0px #000000} span.s2 {text-decoration: underline ; font-kerning: none; color: #0000ff; -webkit-text-stroke: 0px #0000ff}