Good Bone, Bad Bone



For people taking glucocorticoids such as prednisone, the increased risk of bone fracture is a well-documented side effect. Used to treat a variety of medical conditions, including autoimmune diseases and allergies, glucocorticoids are known to cause rapid deterioration in bone strength.
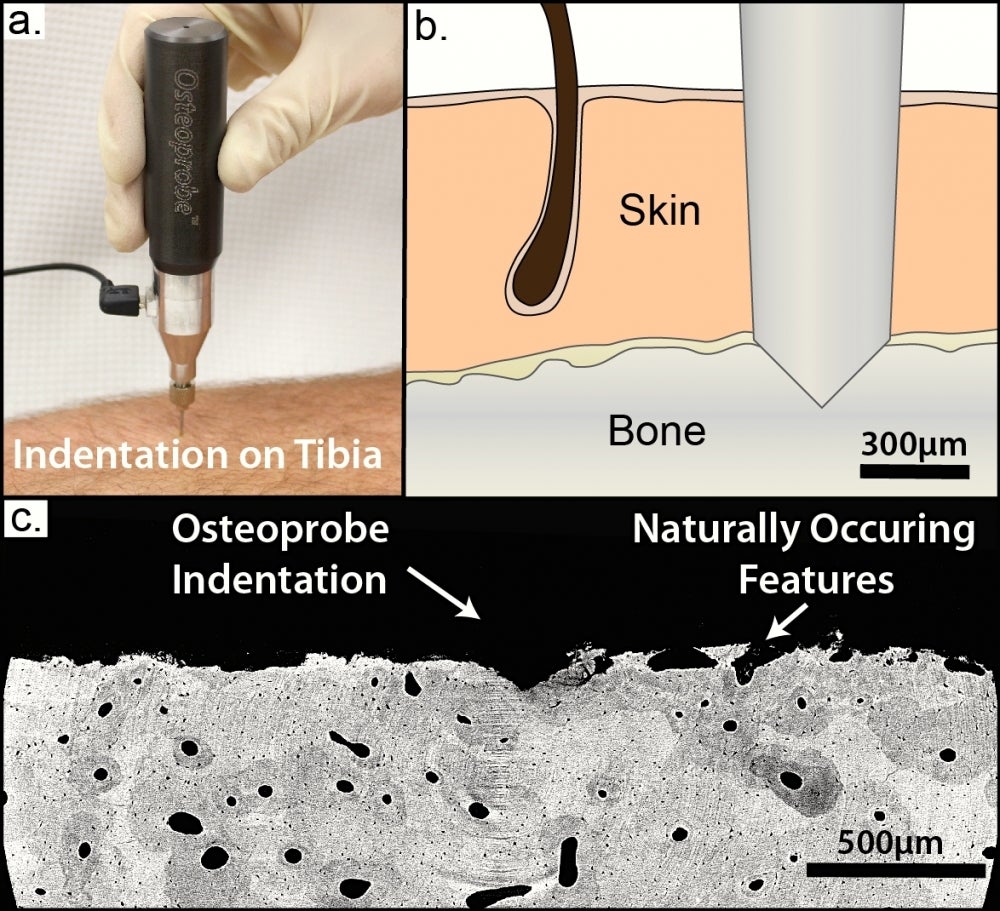
Until now, doctors have been able to measure bone loss — a process that happens slowly, over time — but haven’t had the means for gauging actual bone strength. That has changed thanks to a new hand-held instrument developed in the Hansma Lab at UC Santa Barbara. Called the OsteoProbe, the device uses reference point indentation (RPI) to measure mechanical properties of bone at the tissue level.
A new clinical trial, conducted at the Hospital del Mar in Barcelona, Spain, shows that RPI is sensitive enough to reflect changes in cortical bone indentation following treatment with osteoporosis therapies in patients newly exposed to glucocorticoids. Standard measurement techniques were unable to detect bone changes in this patient population. The trial results are reported in the Journal of Bone and Mineral Research.
“This new paper is a real breakthrough because it’s the first time it’s been possible to do a longitudinal study of bone material properties in patients,” said co-author Paul Hansma, professor emeritus in the Department of Physics. “Up until now, medical professionals have been limited to doing bone mineral density studies, which can take a year or more to show bone changes.”
According to Hansma, measuring bone mineral density (BMD) using today’s standard, dual X-ray absorptiometry (DXA) provides only a partial picture. “DXA measures density, which sounds like a material property but isn’t,” he said. “DXA measures how much calcium bone contains but provides no information about bone quality, and it’s not just how much bone you have that’s important, it’s how good that bone is.”The OsteoProbe works similarly to a center punch — the tool that makes a slight indentation on a surface to indicate the correct placement of a nail. It sets a localized reference point at the bone’s surface that enables precise indentation measurements of bone strength. It was developed by Hansma and colleagues Connor Randall and Dan Bridges, staff research associate and development assistant engineer, respectively, in the Department of Physics.
The instrument is now manufactured for commercial research applications by ActiveLife Scientific, a Santa Barbara company founded by UC Santa Barbara graduates Davis Brimer and Alex Proctor. Brimer and Proctor won the campus’s annual New Venture Competition in 2007 and used the $10,000 prize as startup capital.
About the device
The OsteoProbe measures the bone material strength index (BMSi), which in previously published papers has been shown to be a valuable predictor of bone fracture risk. The index values are similar to percentage scores on an exam. A BMSi of 90 or greater is excellent, 80 to 90 good, 70 to 80 fair, 60 to 70 poor and below 60 very poor.
A study conducted at the Mayo Clinic in Rochester, Minnesota, demonstrated the device’s ability to successfully detect bone quality deterioration in diabetic patients, independent of BMD. In another study conducted at Leiden University in the Netherlands, the tool successfully distinguished between patients with and without fracture, not only in patients with osteoporosis but also in those with osteopenia, the precursor to osteoporosis.
“Bone fracture is becoming more and more of a serious problem as people live longer,” Hansma said. “It’s exciting that it’s now possible to measure BMSi in living patients and hopefully this can guide physicians in the future in choosing appropriate therapies to prevent bone fracture, especially in elderly people.”
Research is ongoing
Exactly how the BMSi relates to the specialized quantities measured by conventional mechanical testing is a focus of current research. In fact, in a recent paper published in the Journal of the Mechanical Behavior of Biomedical Materials, Chancellor Henry T. Yang and two of his graduate students used finite element analysis to investigate the link between BMSi and the mechanical properties of bone itself.
“What’s new in this paper is the ability to correlate indentation measurements from patients’ bones to computer simulations that can predict the strength of the bones,” said Yang, who is also a professor of mechanical engineering. “Such predictions are based on the measured material properties of the bone samples. The results open the door to clinical applications in diagnosis and monitoring, in performing orthopedic surgeries and in developing new therapies.”
The paper’s lead author, Kevin Hoffseth, a graduate student in the Department of Mechanical Engineering, noted that the study results suggest RPI could become an integral part in linking clinical results to the mechanical properties of bone related to its health. “Combining theory and experiment with finite element simulations and indentation testing was an effective approach to study bone indentation and failure — and the link to mechanical properties,” he said.
Clinical trials currently underway in some 20 locations are exploring bone health in a variety of ways. One European study is comparing the bone quality of patients in Norway to that of patients in Spain. People in Norway tend to have higher BMD and a greater frequency of fracture than do people in Spain, Hansma noted.
“That’s the opposite of what it should be if BMD were all that mattered,” he added. “So that means that BMD isn’t all that matters and the hope is that this instrument will reveal the difference in the BMSi between patients in Norway and in Spain.”
Hansma posited that such medical bone diagnostics could become an important feature of future therapeutic treatments. “Now that it is possible to measure whether bone is good or bad in research studies, we can begin learning what diet, exercises, vitamins and pharmaceutical drugs contribute to making bone good,” he said. “After the OsteoProbe gets FDA approval, individual physicians will be able to use it to help them decide about the best therapeutic treatments for their patients.”



