Professor Denise Montell wins second NIH Pioneer Award, receiving $5.5 million for immune therapy research
The National Institutes of Health (NIH) has selected Professor Denise Montell for a Pioneer Award to further develop her work on the innovative immune therapy. The award is part of the NIH’s High-Risk, High-Reward Research program, and comes with $5.5 million of funding over five years. Remarkably, this is the second time Montell has successfully competed for this award, earning her first in 2014. She plans to use the funds to test a new treatment her group is developing for numerous types of cancer and other diseases, such as antibiotic-resistant bacteria.
“The HRHR program champions exceptionally bold and innovative science that pushes the boundaries of biomedical and behavioral research,” said Tara A. Schwetz, NIH Deputy Director for Program Coordination, Planning, and Strategic Initiatives and Director of the Division of Program Coordination, Planning, and Strategic Initiatives, which oversees the NIH Common Fund. “The groundbreaking science pursued by these researchers is poised to have a broad impact on human health”
"It is truly incredible that, for the second time in a decade, Professor Montell has received this prestigious award, which highlights her groundbreaking research and her unwavering dedication to advancing biomedical science,” said Chancellor Henry T. Yang.
“Denise's pioneering work not only enhances our understanding of fundamental biological processes, but opens new avenues for discovery that will benefit countless lives,” he continued. “We are incredibly proud to have Denise as part of our academic family, and as a campus community, we are inspired to continue to push the boundaries of innovation."
Humble beginnings
Montell began her research career by investigating the behavior of a small group of cells in the ovary of a fruit fly. These cells migrate, and she wanted to know how they do it. “Talk about niche,” she remarked. It may be niche, but the system turned out to be a fascinating microcosm into all sorts of cellular behaviors.
“I’m extremely excited about this project because it’s one that really started with my very first graduate student when I was a brand new assistant professor,” said Montell, Duggan Professor and Distinguished Professor of Molecular, Cellular, and Developmental Biology. Her student, Anne Marie Murphy, had discovered that a particular protein called Rac is crucial for border cell migration in fruit fly ovaries. This protein arose early on in eukaryote evolution, and scientists learned that it is nearly universally required for cell migration throughout eukaryotes: from simple protozoa to humans.
But Murphy also made a puzzling observation: A hyperactive form of the protein appeared to be toxic. Expression of active Rac in just a few cells seemed to kill off an entire tissue. “And that puzzled us for a very long time,” Montell said.
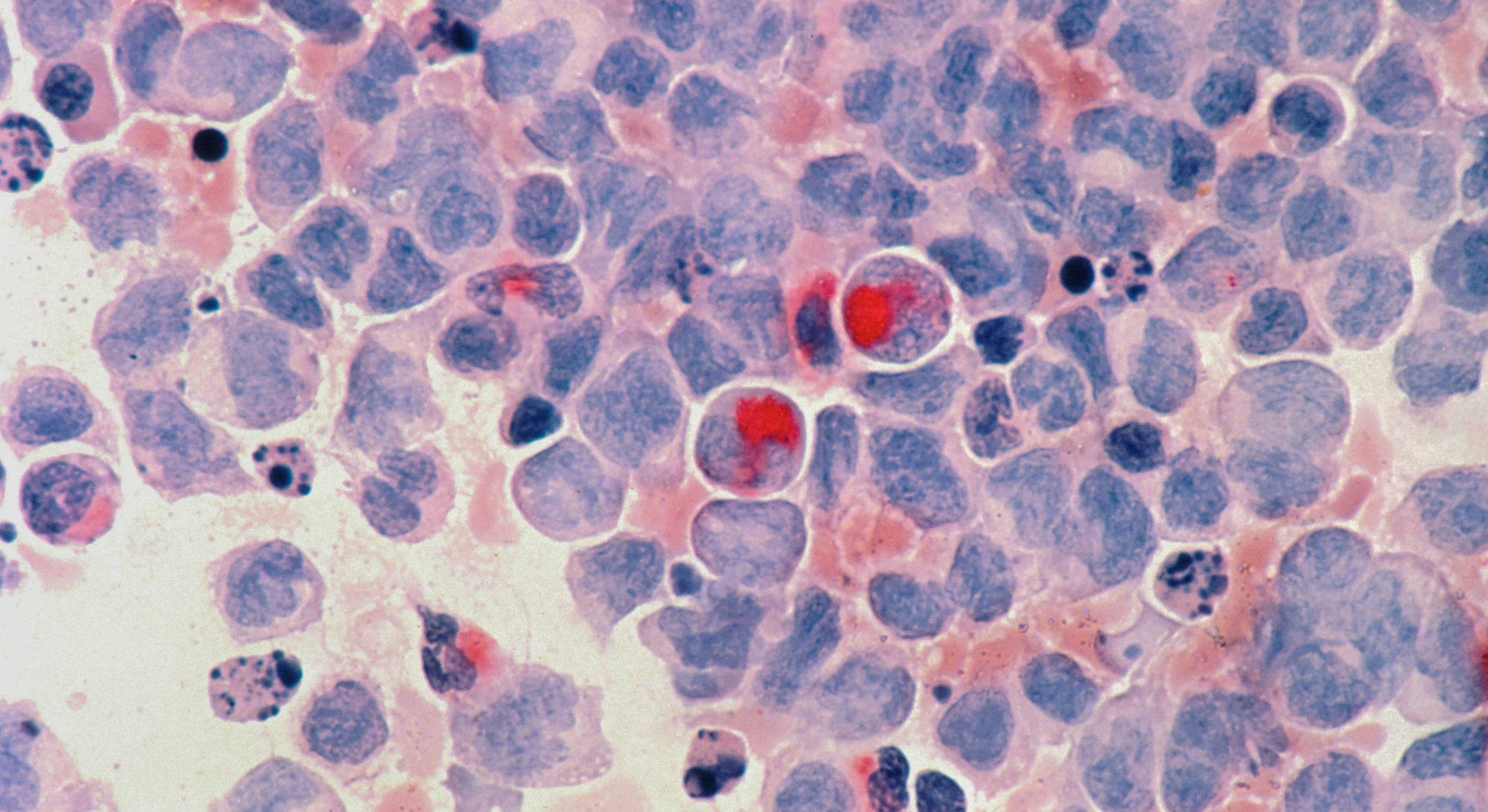
Montell and her group, including project scientist Abhinava Mishra and doctoral student Melanie Rodriguez, recently solved this decades’ long enigma. “Cells expressing active Rac eat their neighbors alive,” Montell said. “It’s wild.” And this phenomenon also occurs in humans with a rare kind of immunodeficiency. Mutated cells with hyperactive Rac eat the individual’s T-cells, which are a central component of the adaptive immune system.
From biological curiosity to biomedical application
The implications of these insights expanded in January 2020, when Assistant Professor Meghan Morrissey interviewed for a faculty position at UCSB. In her talk she explained how she was engineering immune cells called macrophages to eat and kill cancer cells, an approach called CAR-M. After Morrissey joined the university, she and Montell began working to coax the CAR-Ms to consume more tumor cells. They found that adding hyperactive Rac to those CAR-Ms enhanced their ability to eat and destroy cancer cells.
Funding from the Pioneer Award will enable the team to further develop its Rac-enhanced CAR-M (Race-CAR-M) approach. Montell plans to test the technique in mouse models and hopefully advance the technology toward clinical application. She and her colleagues want to understand precisely how active Rac produces this amazing effect. They also want to develop simpler methods to deliver the therapy so that it will be more affordable and accessible.
“I’m tickled that this bizarre observation in fruit flies might ultimately improve cancer treatment,” Montell said.