Treating Vision Loss
Age-related macular degeneration (AMD) affects more than 1.75 million individuals in the United States. Because the population is aging, that number will increase to almost 3 million by 2020. Between 80 and 90 percent of cases in this country are the dry version of the condition, for which no effective treatment exists.
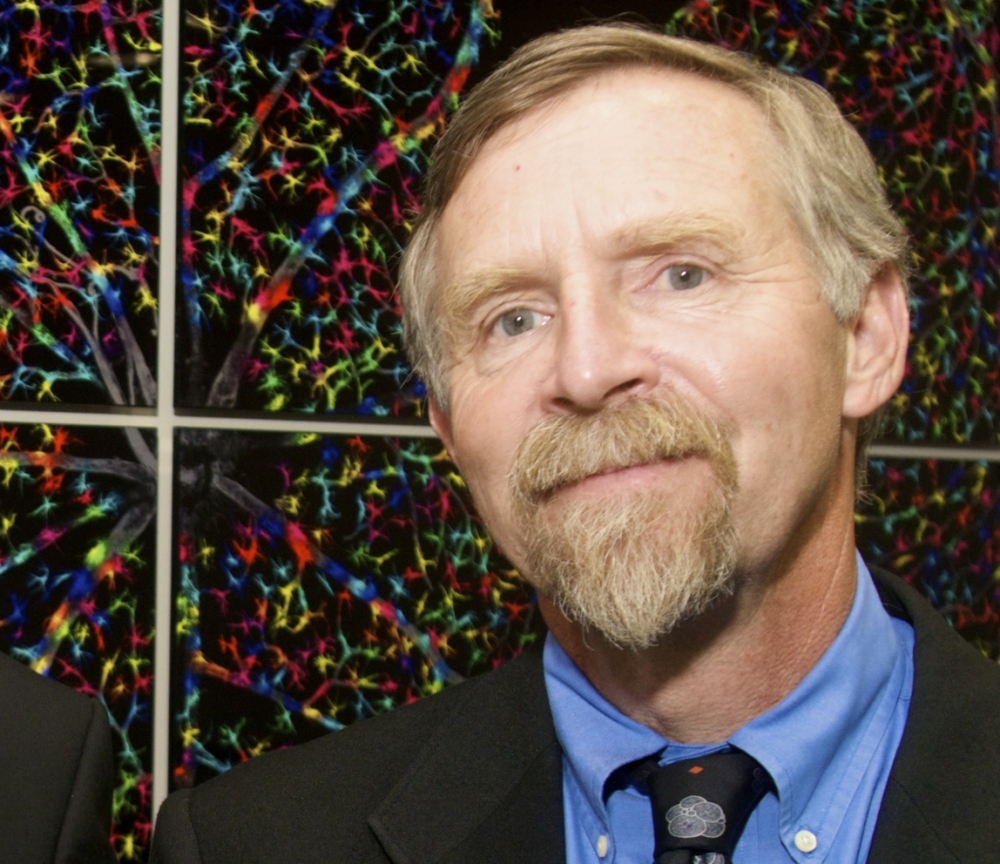
Now, a team of doctors, engineers and scientists — including UC Santa Barbara stem cell researchers Dennis Clegg, Lincoln Johnson, Sherry Hikita and Britney Pennington — has published the preliminary results of a first-in-human clinical trial for dry AMD. Four patients received implants consisting of human embryonic stem cell-derived retinal pigment epithelium (RPE), which support light-sensitive photoreceptor cells critical to vision. The phase 1/2A trial, led by Dr. Amir Kashani, is being conducted at the University of Southern California Roski Eye Institute at the campus’s Keck School of Medicine.
Trial participants have advanced disease with geography atrophy — considered a late stage in dry AMD — and very poor visual abilities. The implant, which was shown to be safe, improved the vision of one patient while the condition of the others remained about the same. The trial results appear in the journal Science Translational Medicine.
This publication comes on the heels of a British clinical trial for wet AMD published last week in Nature Biotechnology.
“Our goal is to implant healthy RPE to revive remaining photoreceptors and prevent any further loss of these light-sensing cells,” explained Clegg, who holds the Wilcox Family Chair in BioMedicine at UCSB and is co-director of the campus’s Center for Stem Cell Biology and Engineering. “Eventually, we would like to be able to provide implants at an earlier stage to prevent patients from losing photoreceptors in the first place.”
In dry AMD, the RPE support cells in the macula become dysfunctional and die. Soon after, the light-sensitive photoreceptors begin to perish. When that happens, clear vision in the direct line of sight is lost while the surrounding vision remains normal.
The implant, which was developed by a team of researchers led by Dr. Mark Humayun of the USC Roski Eye Institute, Dr. David Hinton USC’s Keck School of Medicine and Clegg, consists of a single layer of cells on a synthetic scaffold. Other participating institutions include the California Institute of Technology, City of Hope National Medical Center, CamTek LLC and Regenerative Patch Technologies, Inc. Additional funding was provided by the California Institute for Regenerative Medicine and the Garland Initiative for Vision at UCSB.
“Using advanced imaging methods, doctors can see evidence of integration between the implanted RPE and the host photoreceptors,” said Clegg, who is also co-director of the California Project to Cure Blindness, a collaborative effort aimed at advancing stem cell-based therapy for AMD.
The trial is ongoing and the team continues to analyze more patients. While the preliminary results are encouraging, Clegg said it is still very early in the study.
“We are thankful for the patients that volunteer to do this,” Clegg added. “We explain to them this has never been done before in people. They are almost like astronauts going to the moon for the first time. It takes a lot of bravery on their part.”