Breaking the Code
You may be sensitive to gluten, but you’re not sure. Perhaps you can’t put your finger on a recurring malaise, and your doctor is at a loss to figure it out. A diagnostic method recently developed by UC Santa Barbara professor Patrick Daugherty can reveal — on a molecular level — the factors behind conditions thought to have environmental triggers. By decoding an individual’s immune system, this elegant and accurate method can demystify, diagnose and provide further insight into conditions like celiac disease, multiple sclerosis, preeclampsia and schizophrenia.
“We have two goals,” said Daugherty, a researcher with the Department of Chemical Engineering at UCSB and the campus’s Center for BioEngineering. “We want to identify diagnostic tests for diseases where there are no blood diagnostics … and we want to figure out what might have given rise to these diseases.”
The process works by mining an individual’s immunological memory — a veritable catalog of the pathogens and antigens encountered by his or her immune system.
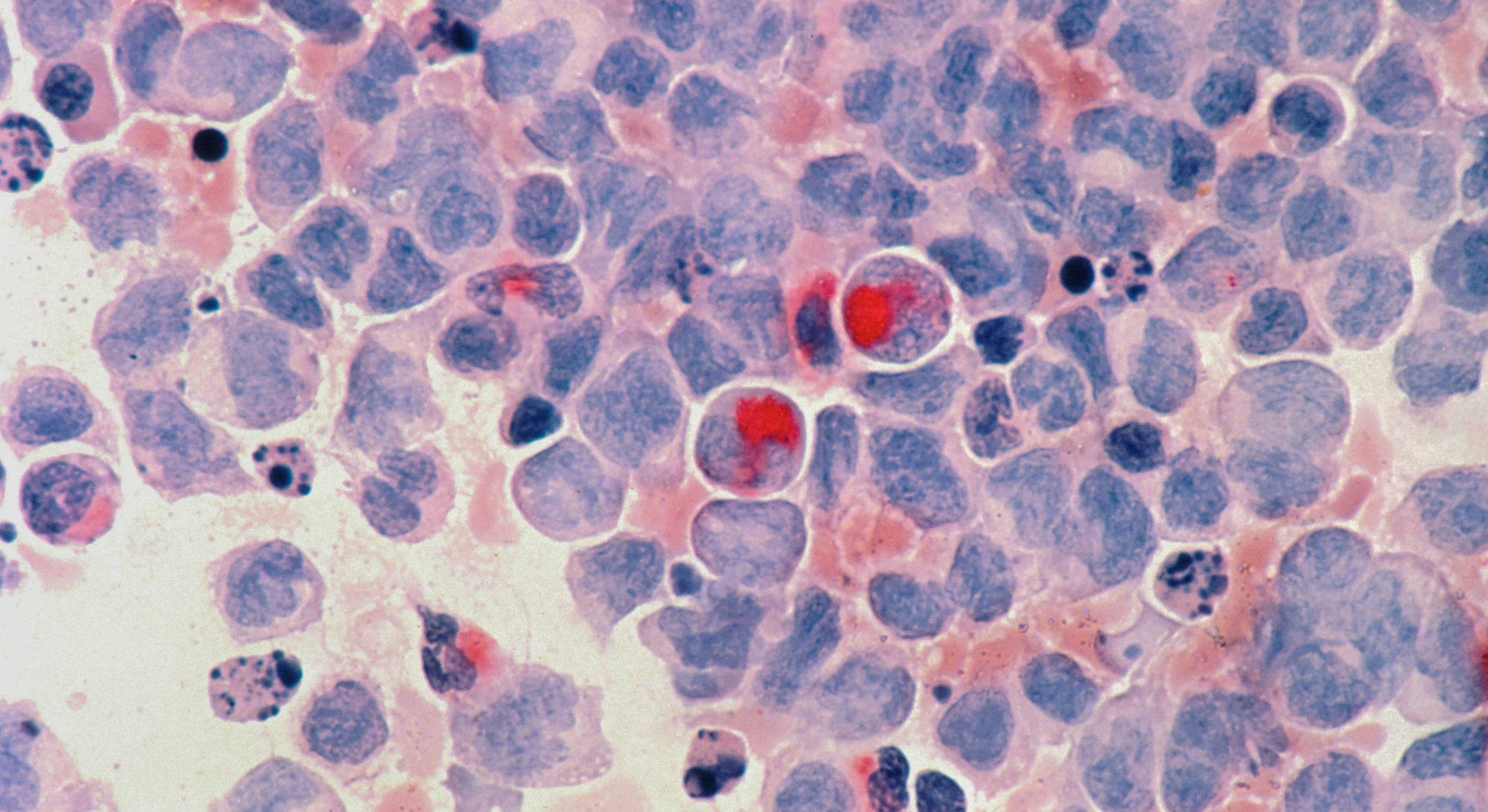
“Every time you encounter a pathogen, you mount an immune response,” said Daugherty. The response comes in the form of antibodies that are specific to the antigens — molecular, microbial, chemical — your body is resisting, and the formation of “memory cells” that are activated by subsequent encounters with the antigen. Responses can vary, from minor reactions — a cough, or a sneeze — to serious autoimmune diseases in which the body turns against its own tissues and its immune system responds by destroying them, such as in the case of Type 1 diabetes and celiac disease.
“The trick is to determine which antibodies are linked to specific diseases,” said Daugherty. Celiac disease sufferers, for example, will have certain antibodies in their blood that bind to specific peptides — short chains of amino acids — present in wheat, barley and rye. These peptides are the gluten that is the root of allergies and sensitivities in some people. Like a lock and key, these antibodies — the locks — bind only to certain sequences of amino acids that comprise the peptides — the keys.
“People with celiac disease have two particular antibody types in their blood, which have proved to be enormously useful for diagnosis,” said Daugherty.
However, sheer variety and number of antibodies present in a person’s blood at any given time has been a challenge for researchers trying to link specific illnesses with specific antibody molecules. One antigen can stimulate the production of many antibodies in response. What’s more, each individual’s antibodies to even the same antigen differ slightly in their form. The idea of using molecular separation to find the disease antibodies has been around for over 20 years, said Daugherty, but no one had figured quite how to sift through the vast amount of molecules.
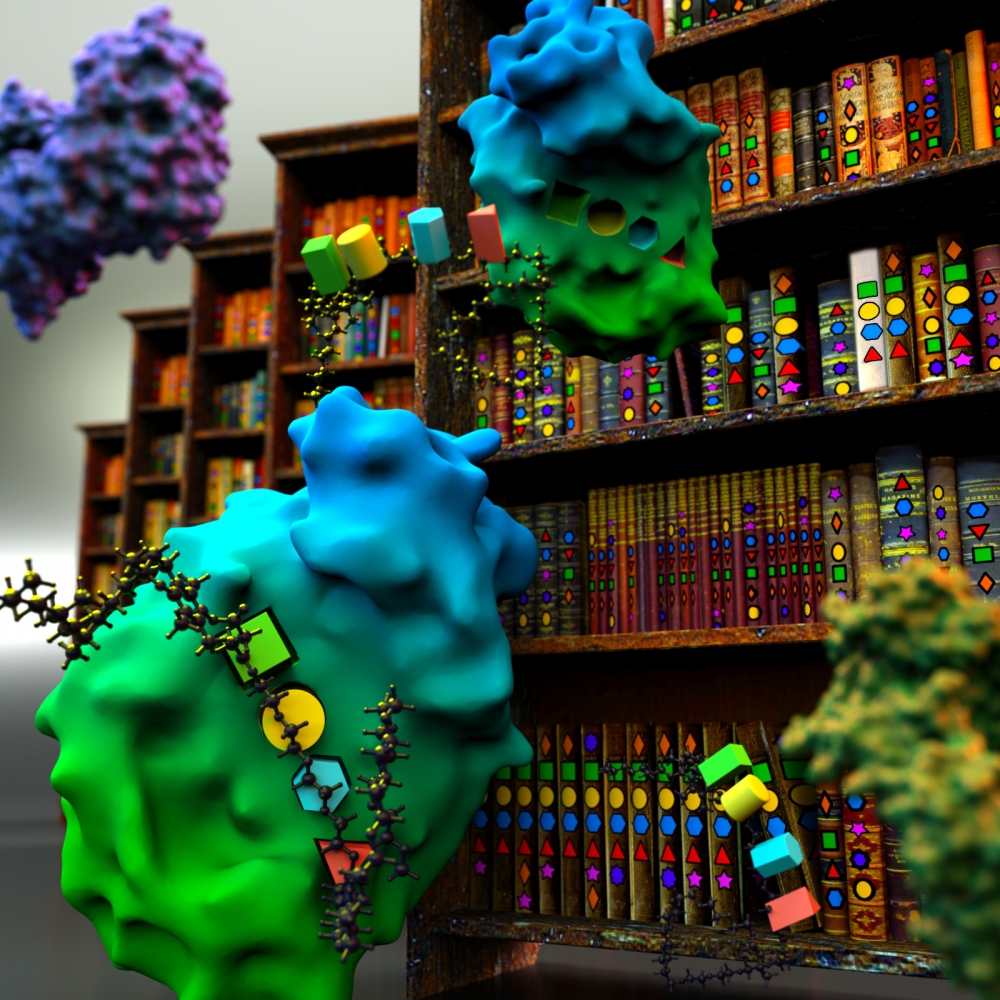
To sort through perhaps tens of thousands of antibody molecules present in a person’s blood, the research team — including John T. Ballew from UCSB’s Biomolecular Science and Engineering graduate program, now a postdoctoral associate with the Koch Institute for Integrative Cancer Research at MIT — mixed a sample of a subject’s blood, which contains the antibody molecules, with a vast number of different peptides (about 10 billion).
“All the keys associate with their preferred lock,” said Daugherty. “The peptides that can bind to an antibody, do so.” The researchers then pull out the disease-bound pairs, in a process that progressively decreases the number of antibodies-peptide pairs that are most unique to a particular disease. Repeated with subsequent patients who may have the same symptoms, phenotypes or genetic dispositions, continues to whittle down the size of the peptide pool. Further in vitro evolution of the best draft peptides can identify the particular sequence of amino acid keys that fit into the antibody locks. This sequence can be used to confirm the antibodies in question as the biomarkers specifically associated with the disease.
“The diagnostic performance of the reagents generated with this approach is excellent,” said Daugherty. “We can discover biomarkers with as little as a drop of blood, and the peptides discovered can be adapted into preferred low cost testing platforms widely used in clinical practice.”
The amino acid sequence of the evolved peptides, when cross-referenced with a database of known proteins, can identify the antigens (that contain the same peptide sequence). This, in turn, can then yield clues into what factors in the patient’s environment may have contributed to the disease. The process may be used to gain insight on diseases that are thought to have environmental triggers, including Type-1 diabetes, autism, schizophrenia/bipolar disorder, Crohn’s disease, Parkinson’s disease, and perhaps even Alzheimers disease. In cases, such as Graves’ disease, where an antibody is identified as the cause (as opposed to simply an indicator) knowing the antibody’s structure can lead to more effective therapies.
“If you can get rid of the antibody, you can treat the disease,” said Daugherty. “By finding these keys, you can block the antibody.”
Research on this study was performed also by partners from the Mayo Clinic; the University of Tampere in Finland; UC San Diego; and Seinäjoki Central Hospital in Finland. Their findings are published in a paper titled “Antibody biomarker discovery through in vitro directed evolution of consensus recognition epitopes,” in the Nov. 11 online issue of the Proceedings of the National Academy of the Sciences.